Recherche translationnelle en santé,
technologie pour la santé et recherche clinique
3D CHIP team / Axis 2 : Bone regeneration and bio-manufacturing of 3D joint models
The reconstruction of large bone defects resulting from severe trauma or tumour resections remains challenging for surgeons. Today, a free flap vascularized fibula is harvested from the patient and transplanted to the reconstruction site (e.g. mandible) but this technique has serious limitations and induces morbidity for patients.
In collaboration with the maxillofacial surgeons of the team 3D CHIP, we are developing an alternative to this autologous bone graft by using biomaterial scaffolds 3D printed and vascularized (see article). These biomaterial scaffolds have a patient-customized shape to fit the anatomy and an internal porosity for bone ingrowth. Pre clinical research has already been conducted to demonstrate the feasibility and efficacy of large bone defect reconstruction under strict ethical regulations. This proof of concept experiments has been funded by patients’ charities (link LFCN) and the European Commission (link Maxibone).
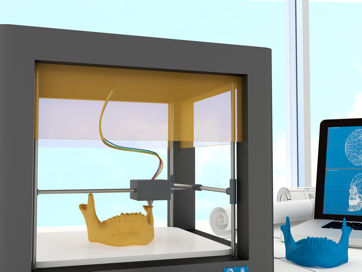
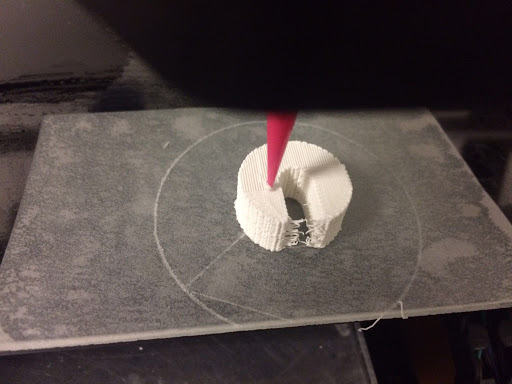
We propose large bone defect reconstructions in one surgical step by using 3D printed and vascularized anatomical biomaterial scaffolds as shown in the following figure.
3D printing of customised biomaterial scaffolds for maxillofacial bone reconstructions
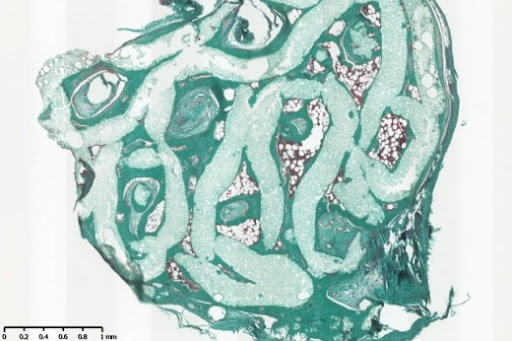
Prior to surgery, angioscanners are performed and medical images are converted to printable stereolithography (STL) files. Anatomical surgical guides and biomaterial scaffolds are 3D printed and implanted in the large bone defects together with a local and axial vascular pedicle. Radiographs, scanners and histology analysis have demonstrated the feasibility of regenerating large bone defects in one surgical step (link to publication). Studies will be conducted to demonstrate the feasibility, safety and efficacy in maxillo-facial reconstructions. A clinical trial aiming at reconstructions in ballistic or cancer resected patients will finally be conducted.
Ageing of the population induces numerous osteoarticular problems such as poly rheumatoid arthritis and osteoporosis. Today, there is no ex vivo model allowing to study the pathophysiology of a human osteoarticular joint. Based on our knowledge of biomaterials and tissue engineering, we propose to bio fabricate a 3D mini-joint.
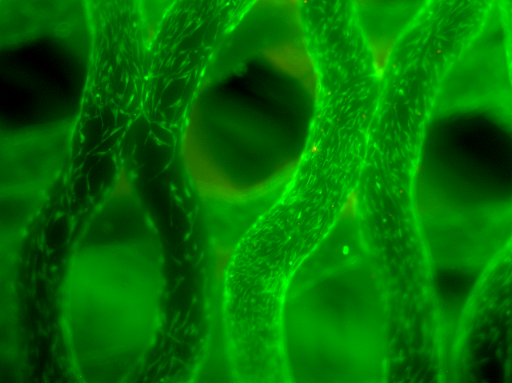
Human mesenchymal stem cells and monocytes will be cultured in 3D photo cross-linkable hydrogels mimicking the natural extracellular matrix of bone and differentiated into osteoblasts and osteoclasts, respectively. Vascularization will be ensured by 3D bioprinting sacrificial bio ink containing endothelial cells. Cartilage micropellets will also be prepared. Articular fibroblasts will be cultured to form a synovial membrane. These tissue structures will be assembled by a bottom-up approach to form a 3D osteoarticular mini joint that can be perfused with drug candidates in ostoporotic bone or inflammatory rheumatology disease models.