Recherche translationnelle en santé,
technologie pour la santé et recherche clinique
iDREAM team / Presentation
Imaging, Development, Repair or REAdaptation, Motor plasticity
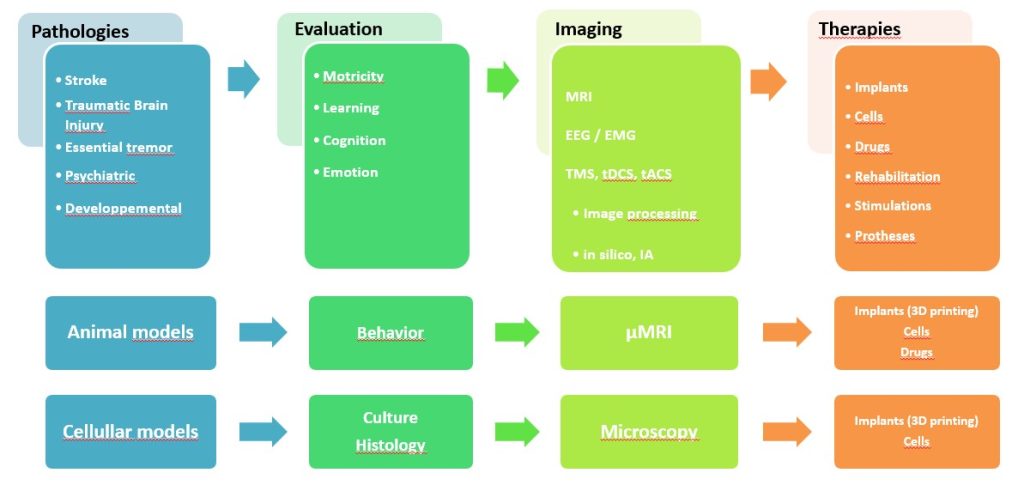
Pathologies: Stroke, Post-traumatic Stress Disorder, Traumatic Brain Injury, Cerebral Palsy, Developmental pathologies
Team leader: Isabelle Loubinoux
co-team leader: David Amarantini
Located at Purpan Hospital, the unit owns a Philips 3T MRI, high density EEG, TMS, tDCS, tACS, Movement laboratory with a Biodex, EEG, EMG, and a safety Level2 cell culture laboratory, a 3D printing laboratory. It has access to the Primate and Rodent animal facilities and to a µIRM scanner (CREFRE).
Therapeutic projects are based on brain stimulation tools and techniques promoting post-injury brain plasticity.
Scientific objectives
All the themes of the iDREAM team share a common focus : understanding the cognitive-motor functions involved in dayly life activities,
through methodological tools for functional exploration, NeuroImaging and NeuroBiomechanics.
We explore therapeutic strategies that will have a major impact on future clinical treatments for acute brain injury and dysfunctions especially in severely disabled patients.
We are driven by a cross-disciplinary and multidisciplinary approach.
We explore the movement from the expert and the healthy individual to the patient.
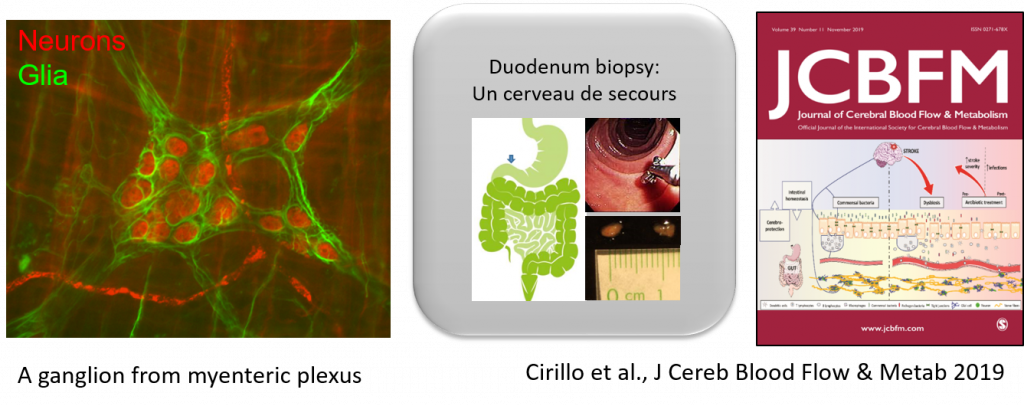
We observe from the neurocellular level to the behavioral level, encompassing the neurological, muscular, psychological, and social levels.
Our research adopts a translational approach, combining fundamental questions with practical applications.
Collaborations
We have a close collaboration with
- the Neurology Department (F. Chollet, JM Olivot, J-F Albucher, N Raposo, A Viguier, L Calvière, M Barbieux-Guillot, J Pariente)
- the Department of Physical Medicine and Rehabilitation (Ph. Marque, E Castel-Lacanal, X de Boissezon)
- the Department of Functional Physiological Explorations (David GASQ)
- the Clinical Investigation Center (O. Rascol, C. Thalamas) and the CIC Biotherapy
- as well as with the Faculty of Sports and Human Movement Sciences of the University Paul Sabatier Toulouse 3 (David AMARANTINI, Julien DUCLAY, Jessica TALLET, Joseph TISSEYRE)
- the Faculty of Sports of INU JF Champollion in Rodez (Camille CHARISSOU, Lilian FAUTRELLE)
Our research axes
The axes explore two types of brain plasticity processes: repair and readaptation.

The team includes scientists in NeuroImaging, Biomechanics and Cell Biology and clinicians in Neurology, Neurorehabilitation, Neurophysiology, Neurosurgery, and Psychiatry.
Our expertises
Our technical skills
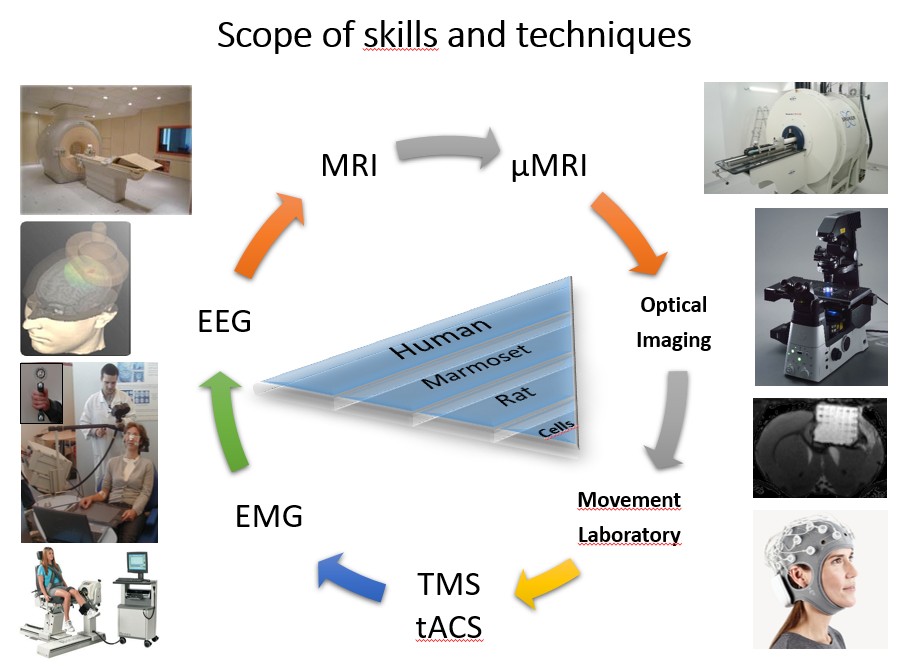
The group’s expertise is highly translational since it ranges from cells, rodents, non-human primates, healthy subjects and patients.
Therapeuties
Our projects must determine the therapeutic strategies that will have a major impact on future clinical treatments for acute brain injury and dysfunctions specifically in severely disabled patients.
They are based on the natural plasticity of the brain and endogenous neurogenesis, and they seek to amplify it by external agents, rehabilitation, non-invasive stimulation, non-pharmacological interventions, drugs, regenerative implants, cellular therapy, neuroprosthesis for prehension allowing functional suppleance.
They also aim to determine the cerebral substrates of these interventions by neuroimaging.
Historically, the team studied Stroke. The leading cause of disability, stroke represents a significant economic cost. Hemiplegia and hemiparesia are the most common deficits. The main result of our previous work is to promote ipsilesional activity.
Them, the team expanded and became more broadly interested in motor disorders such as cerebral palsy, coordination disorders (dyspraxia), neurodevelopmental disorders, and dystonias.
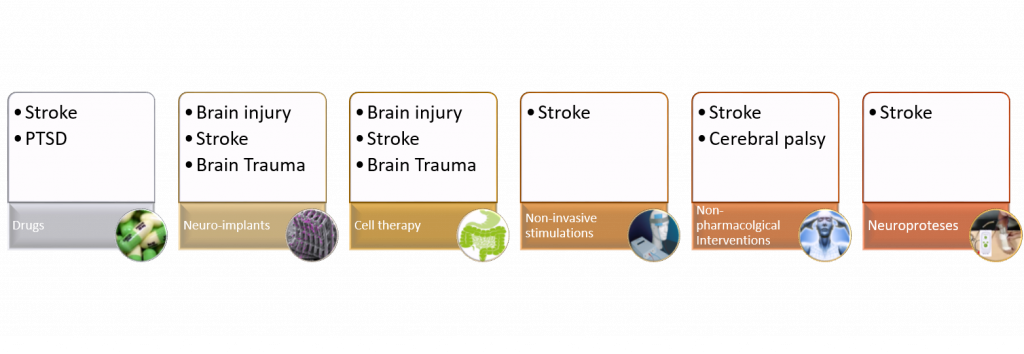
Drugs
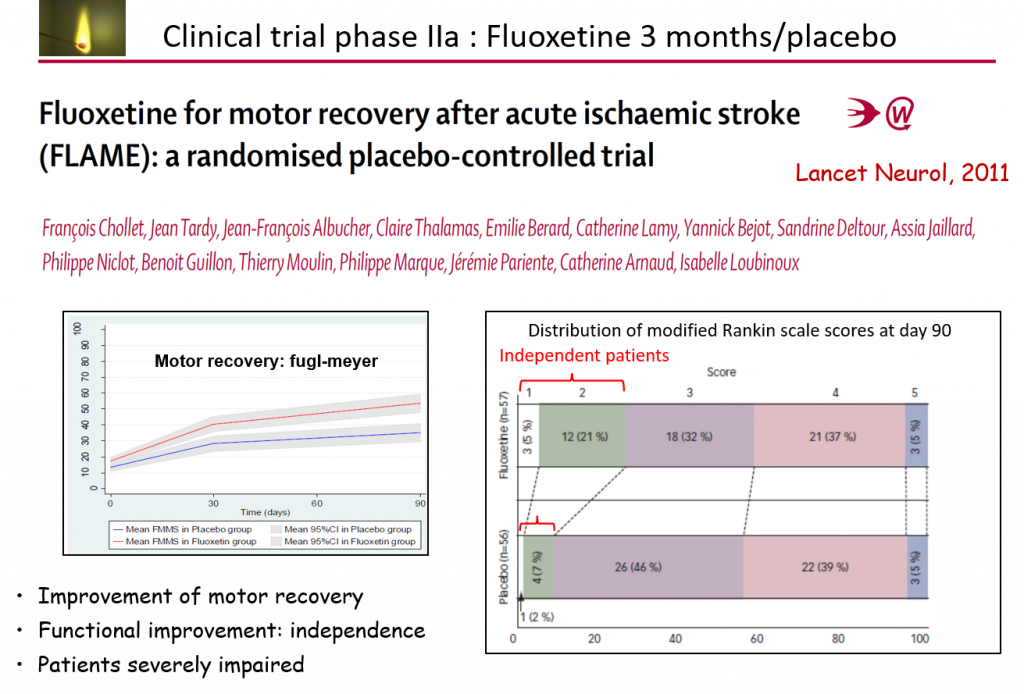
To date, no pharmacological treatment has been validated in human clinics to enhance recovery after stroke.
We have shown that a 3-month treatment with fluoxetine (prozac) significantly increases motor recovery and the proportion of independent patients (Chollet et al. Lancet Neurol 2011). Other studies have corroborated our results (Legg et al., Cochrane Database Sys Review 2019 ; Liu et al., Frontiers Neurol 2021). Large clinical trials testing 6 months of treatment and using low sensitive clinical scales have not shown efficacy.
Neuro-implants
Regenerative medicine brings new hopes lying in neuro-implants (cell therapy and biomaterials) in order to restore long-distance tractus between brain areas. The team made the proof of concept of neuro-implants improving motor performance in rodents. Safety has been demonstrated in the non-human primate (marmoset).
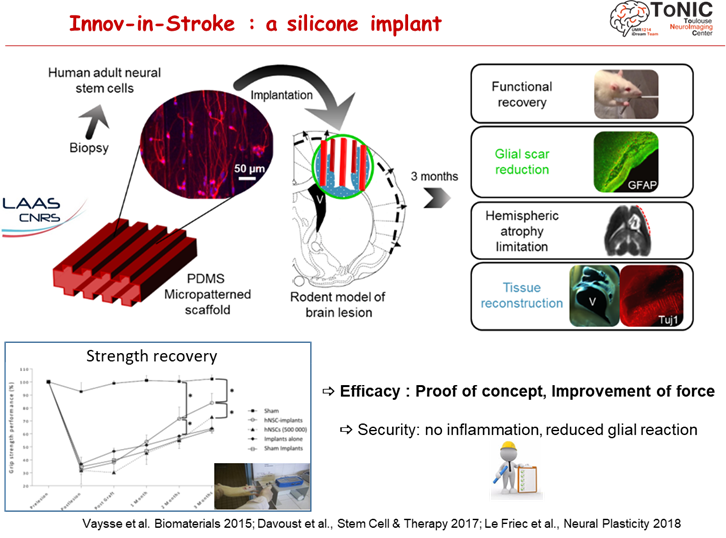
The second generation of regenerative implants focuses on biodegradable implants. 3D printing gives them a comlpex architecture mimicking the cerebral cortex in six interconnected layers.
Non-invasive stimulations
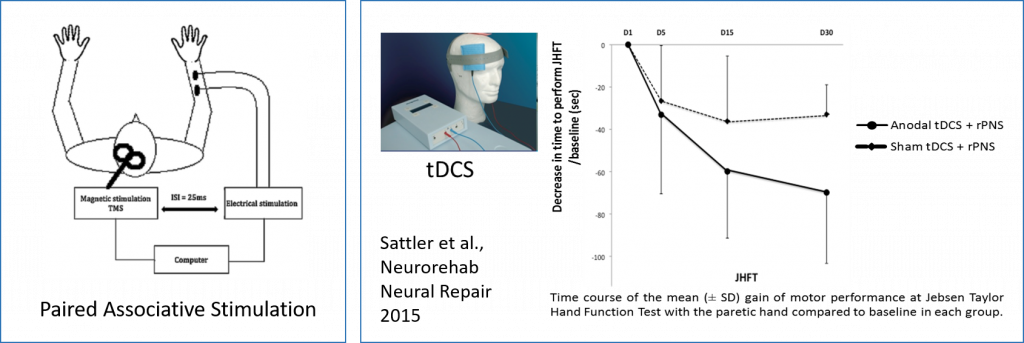
Non-invasive brain stimulations like TMS (transcranial magnetic stimulation), tDCS (transcranial direct current stimulation), or paired associative stimulation (PAS, see figure) that combines peripheral nerve stimulation and TMS have been proposed to promote ipsilesional activity. They can induce long-term changes in excitability of the cerebral cortex to optimize motor recovery in stroke patients. Our team has conducted several studies in this field (Castel-Lacanal E. Ann Phys Rehabil Med. 2015; Sattler et al., Neurorehab Neural Repair 2015; Tarri et al., Ann Phys Rehabil Med 2018).
Non-pharmacological interventions
We are developing projects to test the effects of non- pharmacological interventions in patients with neurological disorders, such as Cerebral Palsy in children and Stroke in adults. The goal of rehabilitation is to improve motor, cognitive and psycho-socio-emotional functioning in order to facilitate the performance of daily living activities and participation in school and social activities. However, to date, it is difficult to advise professionals on the optimal interventions because we lack literature (studies and meta-analyzes) on the effectiveness of rehabilitation protocols.
Our projects aim to test (1) the effects of rhythmic stimuli on procedural learning and (2) the feasibility and effects of rehabilitation programs based on multi-sensory rhythms (ANR grant). In collaboration with the team of Professor Martin Lemay (Director of the Motricity and Cognition laboratory, University of Quebec, Montreal), we are testing the benefits of practicing dance at the motor and cognitive levels (Cherriere et al., 2019; 2020) . In collaboration with Corine Astésano (URI Octogone Lordat, UT2J), the MotRyLang project aims to test the effects of motor rhythm on language acquisition and its disorders during development (Region Grant 2020-2023, C. Astésano and J. Tallet, C. Daigmorte). Ultimately, our work aims to develop re-education practices based on scientific evidence (Evidence-Based Practice) that can feed into the training of professionals involved in re-education.
Neuroprostheses
Following a stroke, less than 20% of patients are able to use the paretic hand in tasks of daily living. Without a therapeutic solution at present, there is a real need to develop on-board functional replacement solutions.
In collaboration with the INRIA CAMIN team (https://team.inria.fr/camin/), we are developing an intuitive and wearable grrasp assistance neuroprosthesis for performing bimanual tasks in daily living.
This project is based on the PREHENS-STROKE study (“Evaluation of the functional impact of a self-piloted grasp neuroprosthesis in the stroke patient”; ID-RCB number: 2020-A01660-39; Sponsor: CHU de Toulouse; PI: David Gasq; funding obtained within the framework of the PHRCi 2019) and the GRASP-AGAIN project (“Development of a wearable grasp neuroprosthesis to restore grasping capacities in daily life after a stroke”).